Battling Childhood Asthma in Missouri Schools
The Missouri Hospital Association (MHA) recently published a series of articles on childhood asthma for its member hospitals. The first focused on the hospitalizations and rate of emergency room visits for children with asthma. The second focused on innovative care models implemented around the state that are improving health, school attendance, and safety for Missouri children with asthma. The American Hospital Association reprinted some of the Missouri asthma intervention case studies in an August 22nd publication, highlighting Missouri’s leadership in addressing childhood asthma.
Missouri KIDS COUNT salutes MHA’s work in bringing attention to children’s health, particularly children dealing with asthma—the leading chronic health problem among children. Building on this work, Missouri KIDS COUNT wanted to expand the story of childhood asthma for our audience.
Introduction
Breathing is an essential function that most of us take for granted, however, for children who suffer from asthma, ‘breathing’ is a central concern that often controls what they do and cannot do each day.
Asthma is a chronic condition that can include coughing, wheezing, and shortness of breath originating from swollen airways—the tubes that carry air in and out of the lungs. Asthma is not curable and treatment primarily focuses on controlling symptoms by following a regular medication regimen and avoiding substances or situations that trigger symptoms. Each person is susceptible to different triggers, which can include allergens (e.g., mold, pollen, and animal dandruff), irritants (e.g., cigarette smoke, air pollution), weather changes, exercise, and respiratory infections.
The life quality of children with asthma depends on how well their symptoms can be controlled. Successfully managing asthma symptoms during childhood, however, is a complex process in which children with asthma, their parents, caretakers, school staff, and health professional must work together to achieve the best outcome possible. Given that children spend a substantial portion of their time at school, it is not surprising that school staff, particularly school nurses, play an essential role in coordinating and implementing asthma control efforts.
In spite of concerned parents and engaged school nurses, many children in Missouri continue to struggle with uncontrolled asthma every day due to expensive maintenance medications and pervasive barriers to quality care.
National Asthma Rates
- Asthma is the leading chronic health problem among children.
- Asthma is the most common cause of children’s absence from school
- An estimated 8.3% of children suffer from this chronic respiratory condition.
- 10.9% of Americans living below 100% of the federal poverty level have asthma, compared to 7.0% of those living at between 100% and 250% of the federal poverty level.
- Nearly one in two children miss at least one day of school each year because of their asthma.
Asthma in Missouri
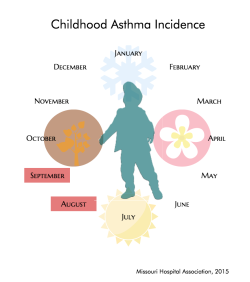
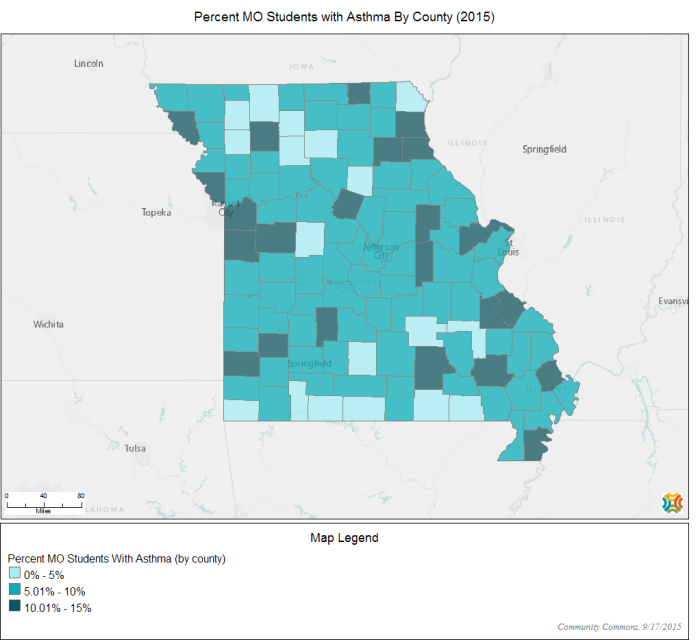
During the 2014-2015 school year, 10%of students enrolled in Missouri’s public schools were affected by asthma. The distribution of childhood asthma, however, varies across the state.
The map below displays the percentage of students diagnosed with asthma per county this year. As can be seen, most counties have asthma rates between 5.1 and 10.0% (medium blue)—which is close to the state average of 10%. A substantial number of counties, however, have rates between 10.1 and 15.0% (dark blue)—which is above the state average. Interestingly, several of the counties with a 10.1 to 15.0% rate were identified by the MHA as hot spots for asthma emergency department visits in 2014, suggesting that children living in counties with higher asthma occurrence are also at risk for having poor asthma control.
In addition, the ratio of school nurses to students (1 nurse per 533 students), which is better than the national average, is still less than what is needed to really have an impact on controlling children’s asthma at school—where they spend so much of their time.
Challenges in Childhood Asthma Control
Children with asthma can have a normal, healthy life with effective treatment and a low-trigger environment. Unfortunately, there are many factors that can get in the way of finding and maintaining effective treatment and an environment that reduces triggers, including:
- Poor medication compliance: Ongoing asthma treatment requires following a strict regimen of controller medications in addition to rescue medication. Many parents and children with asthma do not understand that rescue medication should only be used in case of an emergency, not as the sole treatment for asthma.
- Not being able to recognize symptoms or triggers: Recognizing symptoms requires a level of awareness on the part of the parent, children, and school staff. Also, asthma triggers vary by children, making it difficult to determine the specific substance or situation that might trigger a reaction.
- Not knowing how to use inhalers correctly: Some inhalers can be difficult to use, requiring children to coordinate releasing and inhaling the medication in a timely manner. It is also important that spacers are used to get the maximum benefit from the medication. A spacer is a tube that attaches to the inhaler and holds the medication until the child is ready to breathe it in. Improper inhaler use affects medication effectiveness.
- Poor communication: Proper asthma management requires an ongoing partnership between students, caregivers, school staff, and medical providers. Information exchange among partners is crucial for developing and maintaining effective asthma treatment (for more information, see report by the Brookings Institution).
- Expensive Medical Costs: Asthma is a chronic illness that requires ongoing treatment, which is costly, particularly for families who are uninsured or underinsured. In addition, the health care system, including complicated insurance terminology, can be intimidating and can keep families from accessing medical care regularly—which is crucial for appropriate asthma control.
School Nurses Experience
To provide a more complete picture of the challenges faced by children with asthma and their families, we asked school nurses across the state to share their experiences we us. We would like to express our deepest gratitude to all the school nurses who shared their stories!
Need for better communication
“When parents show up in the emergency room…they are anxious, scared and not hearing or understanding the instructions. Follow-up care the next day is very important…when I follow up [with parents] the next day; it is as though they are hearing the information for the first time. It would be nice to have a system in place to contact the school nurses when the student is discharged from the hospital.”
“Families need to have a primary care provider. This is a critical issue as the student needs a medical home to create that relationship with the physician, family, and school nurse. If they do not have a medical home or do not have a consistent physician to work with, the medication refills do not happen.”
“We had a student riding home on one of the buses who went into an asthma attack…This child did not have any diagnosis of asthma or any medications listed on her health form…The child ended up having such a severe attack that the inhaler did not help—and yet the nurse did not know about this child’s health condition.”
Need for medical equipment and medication
“A mom has three children in the same school…she sent one rescue inhaler for the three children to “share”. A best practice is for each child to have her own inhaler.”
“Rarely, do students bring “spacers” with their inhalers…spacers are very expensive and not covered under certain insurance plans.”
“Many families have issues with getting medication filled or having more than one available for schools, as well as home.”
Relying on nurses as primary care providers
“We have children who come to school asking for ‘treatment’ for their asthma since they don’t have any medication at home. These children are only getting the treatment for asthma symptoms and not the medication and environmental interventions they need to have their asthma managed.”
“Parents rely on nurse’s office to provide nebulizer treatments for their children, even if they have solution and equipment at home.”
Educating students and their families about asthma
“If the child is seen in the ER or Urgent Care, the doctor only gets the ‘acute episode’ under control…does not prescribe the controller medication—which is very expensive, and does not explain asthma in a way the parent can understand that the ‘acute episode’ is being managed by albuterol and that they need additional control medication to manage symptoms.”
“Many of our students are just having their symptoms managed by the ‘rescue’ medication—albuterol. Families go to the ER because they can get quick results—not understanding that this is a chronic condition needing consistent management.”
“Compliance and follow through with a primary care doctor post ER visit are the biggest issues that I face as a school nurse. So little teaching continues to be an issue with ER’s and Urgent Cares. Fortunately most schools have a school nurse to teach students and their families about the physiology of asthma, asthma triggers, the purpose of the different asthma medications prescribed and the importance of using their control medication as directed.”
Asthma and Poverty
Asthma is one of the top five most costly health conditions in the nation. Although effective treatments for asthma have long existed, low-income families often cannot afford treatment. Given that consistent preventive care is crucial for effective asthma control, it is not surprising that children from low-income families continue to struggle with asthma. For instance, last year in Missouri, children living in zip codes with the highest poverty rates accounted for approximately 43% of childhood asthma hospital visits in the state.
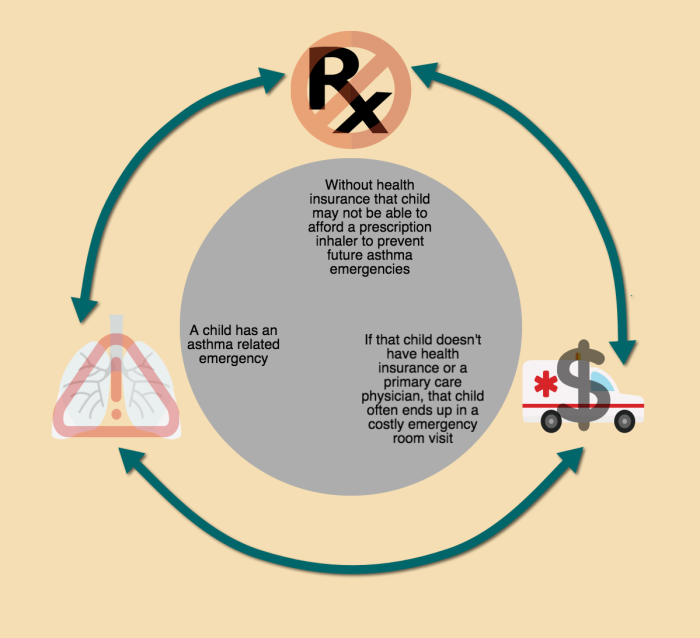
Low-income families may not be able to afford health insurance, may not qualify for Medicaid, and if they have private insurance they can only afford high deductible plans, which may keep them from regularly accessing preventive medications and medical care. The lack of preventive care, in turn, can lead to a higher occurrence of asthma related emergencies. Costly emergency room treatment can cause further financial strain, which can keep low-income families in a never ending cycle of not being able to afford preventive care.
Uncontrolled asthma has been associated with higher school absenteeism. In a recent report by Attendance Works, featured in the St-Louis Post Dispatch, school absenteeism was directly tied to health factors, including asthma. School absenteeism was particularly high among students who were eligible for free lunch— a marker of poverty. School absenteeism place low-income children at-risk for experiencing academic difficulties and further contribute to current achievement gaps.
Efforts to Promote Childhood Asthma Control
As summarized in a recent article by the MHA, Missouri has outstanding programs that follow innovative approaches to improve the life quality of children with asthma. In this section we highlight some evidence-based programs involving the participation of school staff, particularly school nurses. In addition, we note recent legislation and a newly funded program that positively affect the care of children with asthma.
The Missouri Asthma Prevention and Control Program (MAPCP)
The MAPCP has promoted partnerships between public and private organizations with the purpose of improving the life quality of children with asthma. Some of their most notable accomplishments include: the development and distribution of the Missouri School Asthma Manual, training school nurses to deliver self-management education, and demonstrating the effectiveness of multi-faceted, community-wide interventions for improving asthma care. Guidelines developed by the MAPCP have served as a foundation for the development of programs aimed at improving asthma care for children.
Multifaceted Intervention at Kennett Public Schools (KPS)
Following a partnership model, school nurses in KPS developed and led an intervention with several components including: self-management education, assessment of asthma severity, home environment assessments, specialist referrals, and fostering connections between health care providers and caregivers. This program improved asthma control as indicated by fewer asthma symptoms and a reduction in childhood asthma hospitalizations. School nurses attributed the success of the program to various factors such as regularly sharing health information with care providers, prompting providers to adjust medication, teaching parents about asthma management, monitoring adherence to asthma controlling medications, and teaching students the skills to self-manage their asthma.
Teaming Up for Asthma Control (TUAC)
MAPCP in partnership with the University of Missouri Asthma Ready Communities created TUAC, a program in which school nurses served as the center of the intervention. School nurses received training in three main areas: (1) asthma severity assessments, (2) evaluation of student self-care behaviors, and (3) teaching students and their families about asthma. Participation in this program resulted in better asthma control in participants as indicated by lower ER visits and hospitalizations, which in turn resulted in lower healthcare costs.
TUAC Success Stories:
A student with asthma and multiple allergies had to visit the health office daily to use his rescue inhaler, sometimes more than once a day! He did not use his preventive inhaler regularly, did not know how to use his inhalers correctly, and had parents who smoked. Within a few sessions, he learned how to use his inhalers correctly and started using his preventive inhaler daily (as he was supposed to). His parents started smoking outside and Dad decided to quit smoking altogether. The student no longer visits the health office to use his rescue inhaler!
A student with asthma had visited the ER many times over the last couple of years because of breathing problems. Although she had asthma for a while, she did not know how to use her inhalers appropriately. After only two sessions, she learned how to use her inhalers correctly! Through great communication, her mom and school nurse realized that she needed to see a doctor to change her medications. Proper inhaler use and the right medications helped this student to control her persistent asthma within a few days!
Childhood Asthma Rescue Education (CARE) Barton County Memorial
The goal of this program is to educate children, families, health professionals, and the general public about asthma as a chronic condition. The program is implemented by Certified Asthma Educators who work in combination with medical care providers and school nurses to ensure the proper use of medical equipment and promote self-management skills. CARE also conducts home evaluations to identify asthma triggers.
BREATH (formerly Project Concern)
The Asthma and Allergy Foundation of America, St. Louis Chapter, created BREATH to provide medical assistance for uninsured and underinsured children. The program provides life-saving asthma and allergy medications, equipment, education, and support. They serve families, schools, and nurses all over the Greater St. Louis area.
Administration of Asthma Rescue Medication to Students and MO HealthNet’s New Education and Environmental Assessment Program
In 2012, the Missouri Legislature, in collaboration with the St. Louis Chapter of the Asthma and Allergy Foundation, passed House Bill 1188 (RSMo 167.635), which authorizes a school nurse to maintain a supply of asthma-related rescue medication, and to use such medication on any student believed to be having a life-threatening or acute asthma episode. This effort to improve asthma care was featured in a recent article by the Center for Health Policy at the Brookings Institution. While no funding was allocated by the General Assembly for the purchase of rescue inhalers, many school nurses and districts have found ways to stock this life-saving treatment medication.
Even more exciting for children with asthma and their families, the state’s Medicaid division, MO HealthNet, is in the process of implementing a statewide asthma education and in-home environmental assessment program for MO HealthNet enrolled youth. Evidence has shown that the combined approach of asthma education and in-home environmental assessments lead to better health outcomes in the youth population.
The program will focus on youth with a primary diagnosis of asthma and evidence of a high risk of uncontrolled asthma as indicated by one or more of the following: multiple inpatient hospital stays, multiple emergency room visits, multiple urgent care visits, overuse of rescue inhalers, and/or use of inhaled corticosteroids as a maintenance medication. MO HealthNet’s program will provide both asthma education sessions with a national and/or certified asthma educator and in-home environmental assessments by nationally and/or state certified environmental assessors. A physician prescription will be needed in order to obtain the services in the program.
Conclusions
“The front-line soldier in the asthma control battle is often the school nurse.”— Herb Kuhn, MHA President and CEO
Providing children with the resources needed to learn how to control their asthma symptoms can radically improve their overall health. In addition, improvements in health outcomes are likely to reduce school absenteeism and improve academic performance.
Children with asthma need help learning to manage their condition. As suggested by the programs reviewed, efforts that involve the participation of families, school staff, and health professionals are the most effective. As discussed in a recent report by the Center for Policy at the Brookings Institution, improving childhood asthma outcomes will require greater coordination of clinical, non-clinical, and community resources.
School nurses are critical players in fostering and maintaining collaborations as well as coordinating asthma treatment efforts. Given the importance of school nurses in treating chronic illnesses, our next feature will focus on their efforts to keep our children healthy.
The Annie E. Casey Foundation recently released the 2015 KIDS COUNT Data Book, ranking every state on child well-being measured in four domains. This year, Missouri ranked 26th overall, but 33rd in health, the lowest of the four domains evaluated for the state, which also include family and community, education and economic well-being.
We thank everyone who contributed to this feature, particularly school nurses who are on the front lines of child well-being and health every day, and the committed experts at the Missouri Department of Health & Senior Services, Peggy Gaddy, Asthma Program Coordinator and Marjorie Cole, State School Nurse Consultant.
Asthma Prevention and Control
Asthma and Allergy Foundation for America (AAFA)
Learn How to Control Asthma (CDC)
Environmental Protection Agency (EPA)
For more information on efforts in Missouri to fight asthma cost, see article from Aligning Forces for Quality
Video Recommendation: Watch school nurse, Lizzie Crockrell, share her experience helping children to control their asthma symptoms
Does Race Increase Your Chance of Asthma? – written/created by Nursing@USC, the online FNP program
This piece delves into black children being diagnosed with asthma twice as often as white children, as well as identifying risk factors and the impact asthma has on school attendance.
September 22, 2015